PRP – Platelet Rich Plasma Therapy
What is Platelet Rich Plasma?
Platelet Rich Plasma therapy (PRP) is a groundbreaking non-operative treatment option that relieves pain by naturally promoting long lasting healing of musculoskeletal conditions. The platelets in your blood carry natural healing properties that help your body repair damaged tendons and soft tissue. They decrease inflammation, assist with cell growth/healing, and alert your immune system while also strengthening tissue.
Medical practitioners can use platelet rich plasma (PRP) injections to promote the healing properties of your own blood to help the body repair soft tissue damage. Currently, a growing number of people are turning to PRP injections to treat an expanding list of orthopedic conditions, including osteoarthritis. It is most commonly used for knee osteoarthritis, but may be used on other joints as well.
How is it done?
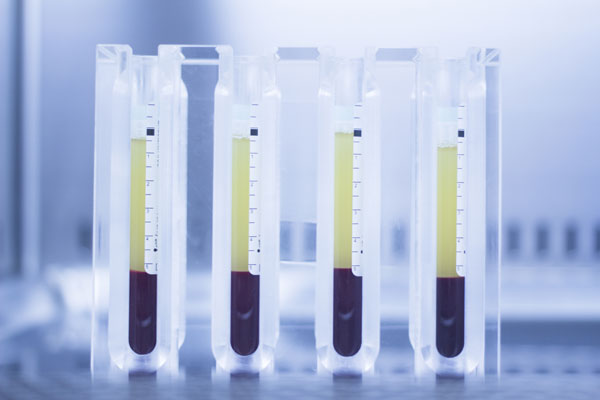
PRP begins by collecting blood from the patient similar to a clinic laboratory blood draw. The amount of blood needed is determined by the size of the area to be treated and the concentration of platelets desired. The blood is then placed in a centrifuge where it is separated into 3 components, the plasma portion of the blood, the PRP layer, and the cellular layer containing red and white blood cells. The PRP layer is then extracted to be used for injection.
PRP injections are completed using visualization techniques via ultrasound or fluoroscopy, so that the injection is administered exactly to the injured area of the body. Local anesthetic can be used at the site of the injection to minimize patient discomfort.
The patient is educated about activity restrictions and is often recommended to limit activity and WB for the next few days. The patient is encouraged to rest the area for a few weeks and then will begin the rehabilitation process following the procedure.
The patient is typically seen by the physician in the clinic for routine follow-up about 1 month after the injection.
The injections are completed as an outpatient procedure, and patients return home the same day. Additional injections may be needed depending upon how the tissue reacts to the initial PRP injection, you may need an additional injection. An evaluation will be done to see if the tissue is responding before a second procedure is planned. Your treatment plan will be discussed in detail following your injection.
What to expect after a PRP injection
Following the injection the injection site may become swollen and painful. This will hopefully replace chronic inflammation with a short period of acute inflammation and will also stabilize the tissues in the affected area. The area may be aching and throbbing for at least 24 hours, and this could last for up to 7-10 days. Tylenol or your prescribed pain medication can be used for post injection pain. Most patients begin see benefits approximately 4-6 weeks post injection.
Pre-Care and Post-Care Instructions for PRP treatment
Click on the headings below for additional information concerning pre- and post-care instructions to prepare for blood draw and PRP treatment.
Pre-Care Instructions to prepare for blood draw and PRP treatment
The American Academy of Orthopaedic Surgeons recommends patients adhere to the following pre-injection guidelines:
- Avoid corticosteroid medications for 2-3 weeks prior to the procedure
- Do not take anticoagulation medication like Coumadin/Warfarin, Plavix/Clopidogrel for 5 days before the procedure. (discuss with physician before discontinuation)
- Stop taking non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, Motrin and Aleve, or arthritis medications such as Celebrex, a week prior to the procedure
- In addition, high doses of some Vitamins and Supplements like Omega 3s can thin your blood so please avoid these
- Drink plenty of fluids the day before and day of the procedure
- You should not have PRP therapy if you have: Abnormal platelet function, Active systemic infection, Active cancer, Low-platelet count, Severe anemia, Hypofibrinogenaemia
During the course of your treatments, notify our staff of any changes to your medical history, health status, or personal activities that may be relevant to your treatment.
Post-Care Instructions after a PRP treatment
What to Expect after Treatment:
Immediately following the procedure, the most commonly reported temporary side effects are soreness, redness, swelling, tenderness, numbness and/or a feeling of pressure at the injection sites and/or treated area(s).
Discomfort/ Pain Management:
Cold gel packs/ice may be gently applied immediately after treatment to reduce swelling if needed. Tylenol and or prescriptions pain medication is recommended if needed for discomfort but avoid NSAIDs such as ibuprofen, Motrin and Aleve.
To Maximize Results and Prevent Complications:
- Keep moving the joint and stretching with gentle active range of motion (AROM) exercises
- Avoid strenuous exercise, heavy lifting, or impact activity for 1 week
- Transition with non-impact activities with progressive resistance, duration, and intensity: elliptical trainer, stationary bike, deep water running before resuming full exercise regimen
Follow up Appointment/Treatment:
Most patients see improvement within 4-6 weeks with continued improvement for up to 12-16 weeks depending on the area treated. If the desired level of pain relief has not been reached within 4 weeks we recommend repeating the procedure at 4-6 week intervals until you achieve the result you desire for up to 3 treatments
PRP Common Treatment Areas
Click on the common treatment areas below for additional information on the various conditions PRP can be used for to treat pain.
Neck
- Whiplash injuries
- Headaches related to the neck arthritis
Back
- Lower back pain
- Facet joint arthritis
- Pain associated with scoliosis
Shoulder
- Arthritis
- Rotator cuff tendinitis or tear
- Rotator cuff impingement syndrome or Bursitis
- Bicipital tendinitis
- Labrum tears
- Arthritis
- Instability
Elbow
- Arthritis
- Bursitis
- Lateral epicondylitis (Tennis Elbow)
- Medial epicondylitis (Golfer’s Elbow)
- Common extensor tendon injuries
- Bicep tendon injuries
- Triceps tendon injuries
Wrist/Hand
- De Quervain’s tenosynovitis
- Arthritis
- Other wrist or finger tendinitis
- Ligament tears or dysfunction of the fingers and tendon
- Ligament or cartilage damage
Hip
- Arthritis
- Iliotibial band tendinitis (ITB Syndrome)
- Psoas tendinitis and bursitis
- Greater trochanteric bursitis
- Hip labrum tears
- Piriformis syndrome
- Sacroiliac joint dysfunction
Knee
- Arthritis
- Patellar tendinitis (Jumper’s Knee)
- Patella femoral syndrome
- Chondromalacia of the patella
- Partially torn or strained major ligaments of knee (ACL/LCL/MCL)
- Meniscus tears
- Patellar instability
Ankle/Foot
- Plantar fasciitis
- Achilles tendinitis
- Peroneal tendinitis
- Arthritis
- Recurrent ankle sprains
- Other foot or ankle tendinitis conditions